It astounds me how the progression of an idea works. I mentioned this in an earlier post but I think it's worth noting again. Somebody at some point looked at a calf getting milk from its mother and thought, "hmmm, I wonder if we could drink that." The same applies to other things like coffee and chocolate - "Let's do these 19 steps to this bean and we might have something good in the end." The discovery of something new and the progression of how it got to that point intrigues me. Somewhere along the line, someone witnessed what happens when an electrical charge is given to the brain. They applied that information to invent a procedure that today has been performed over 250,000 times. Amazing.
There are plenty of sites that describe what Deep Brain Stimulation (DBS) is and how to take one for a test-drive. I thought I would do something a little different and tell you about it from the perspective of someone going through it. Namely...me.
How the thought of DBS even got in the discussion.
I always thought DBS was in my future. I figured by the 10-year mark of my diagnosis my symptoms would progress enough and the technology would advance enough for me to have the surgery. Well, here I sit at the 5-year mark contemplating DBS pros and cons. In my last PPMI visit with my neurologist, Dr. Richard, and her assistant Paul DeRitis at the Univerisity of Rochester, we discussed the dystonia (distortion) and bradykinesia (slowness) still hindering my left hand. On medication, my hand will open and close albeit VERY slowly making it difficult if not impossible to use. Fine motor skills like picking up screws or nails to work around the house cannot be done. Off meds, my hand curls closed like a hook and is useless. Our discussion centered around my medication regime and if there was anything else that could be adjusted. I'm maxed out on Carbidopa/Levodopa as any more and I start to get the rolling wave of dyskinesis starting with my head and working its way down to my torso. Nothing on the scale of Michael J Fox but dyskinesis none the less. Other Parkinson's meds are a no-go due to the side effects associated with impulsivity. So Botox was mentioned. The premise here is there are two muscles involved in most movements. One pulling and one relaxing - think bicep verses triceps. The thought is to inject Botox into the muscle of my hand to relax it so it won't form my hand into a hook. A couple of problems with this procedure: One - it only lasts a few months and you have to get reinjected. Two, it weakens the muscle. I'm already struggling opening things like Ziploc and Potato chip bags. If this makes it worse I'll really be in trouble. I wasn't getting a good feeling about this procedure so I asked what else we could do. This is where they suggested I consider DBS surgery.
DBS appointment - Step one
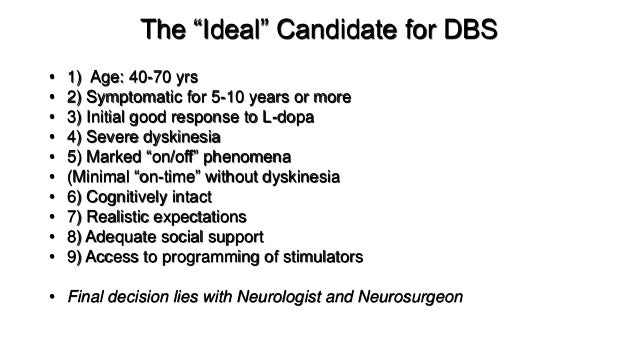
With the anticipation of going down the DBS route, I get to add another neurologist and now a neurosurgeon to my repertoire of medical professionals. Dr. Richard and Paul are phenomenal and if you're near upstate NY I highly recommend you seek them out. However, now I get to deal with another highly regarded movement disorder specialist, Dr. Burack also of the University of Rochester. The new neurologist works in tandem with the neurosurgeon to perform the DBS surgery. While the surgeon is doing the cutting and insertion of the electrodes, the neurologist is directing the precise location and final placement. I'm getting ahead of myself though. Step one is to meet with the new neurologist to see if you qualify for surgery. Apparently, to qualify for DBS you have to meet certain criteria.
This is a suggested list, not a hard and fast rule. Some places have their own criteria or worksheets to determine if you qualify. The University of Florida has a multi-part form that is graded to see your probability of being a good patient. (here) I can understand why they require you to be physically ready for the surgery, but I was not expecting all the questions on the mental readiness part. Number 7 (above) Realistic expectations? Would the surgery not work as well if I expected it to do more for me? Number 8 - adequate social support- why? To keep me from getting depressed if it doesn't work as well as expected? There may be some side effects of this operation that I need to dig into more.
So after a couple hours of questions and a brief exam the neurologist determined that I qualify to move on. Step one, check, but I'll have to go back and ask her how realistic my expectations were.
Next up - Step Two - an MRI and examnation off medication.